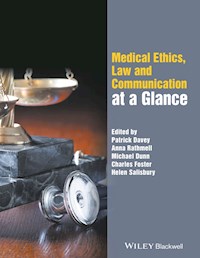
Medical Ethics, Law and Communication at a Glance ebook
149,99 zł
Dowiedz się więcej.
- Wydawca: John Wiley & Sons
- Kategoria: Biznes, rozwój, prawo
- Język: angielski
Medical Ethics, Law and Communication at a Glance presents a succinct overview of these key areas of the medical curriculum. This new title aims to provide a concise summary of the three core, interlinked topics essential to resolving ethical dilemmas in medicine and avoiding medico-legal action. Divided into two sections; the first examines the ethical and legal principles underpinning each medical topic; while the second focuses on communication skills and the importance of good communication. Medical Ethics, Law and Communication at a Glance offers an accessible introduction to the fundamentals of good medical practice, and will provide indispensable support for undergraduate medical students and nurses, as well as newly qualified healthcare professionals.
Ebooka przeczytasz w aplikacjach Legimi na:
Liczba stron: 322
Rok wydania: 2016