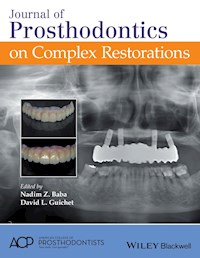
Journal of Prosthodontics on Complex Restorations ebook
0,0
339,99 zł
339,99 zł
-50%
Zbieraj punkty w Klubie Mola Książkowego i kupuj ebooki, audiobooki oraz książki papierowe do 50% taniej.
Dowiedz się więcej.
Dowiedz się więcej.
- Wydawca: John Wiley & Sons
- Kategoria: Biznes, rozwój, prawo
- Język: angielski
Journal of Prosthodontics on Complex Restorations compiles 34 of the journal's best articles discussing complex restorative dental challenges, collecting notable works on the subject. * Presents a curated list of the best peer-reviewed articles on complex restorations from the pages of Journal of Prosthodontics * Covers management of maxillofacial defects using CAD/CAM technology, tooth wear, congenital disorders, orthodontic/prosthodontic patients, patients with surgical and maxillofacial challenges, and completely edentulous patients using new ceramic material * Offers a mix of clinical reports, research articles, and reviews
Ebooka przeczytasz w aplikacjach Legimi na:
Liczba stron: 648
Rok wydania: 2016
0,0
Oceny przyznawane są przez użytkowników Legimi, systemów bibliotecznych i innych serwisów partnerskich. Przyznawanie ocen premiowane jest punktami Klubu Mola Książkowego.
Legimi nie weryfikuje, czy opinie pochodzą od konsumentów, którzy nabyli lub czytali/słuchali daną pozycję, ale usuwa fałszywe opinie, jeśli je wykryje.